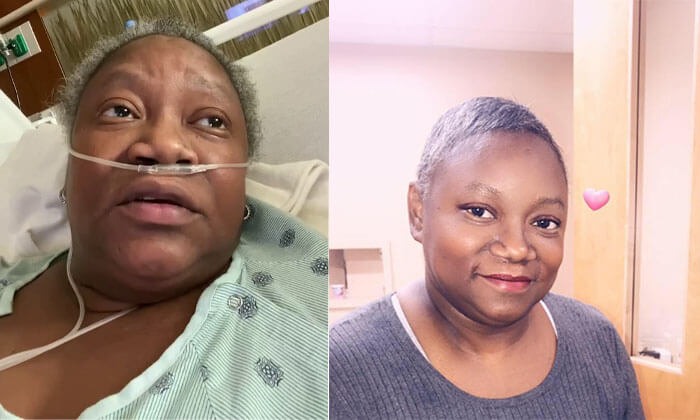
Dr. Susan Moore, MD was a 52 y/o family medicine/geriatric medicine specialist in Indianapolis, IN. Born in Jamaica, Dr. Moore grew up in Michigan, receiving her medical degree from the University of Michigan Medical School in 2002.
Dr Moore tested positive for the coronavirus on November 29 and had symptoms of a high respiratory rate, high heart rate, high fever and coughing up blood. On December 4, she was admitted to IU Health North Hospital in Carmel, Indiana where she received substandard care which she posted to Facebook and her story has gone viral.
Her accusation of the lack of care was because she was black. I want to add a second macabre reason. But first, let’s review her story.
First, she was no stranger to the challenges of getting proper medical care. She had sarcoidosis, an inflammatory disease that attacks the lungs, was frequently treated at hospitals and nearly every time she went she reportedly had to advocate for herself just to get baseline, proper care.
In her Facebook video from the hospital with COVID, she described the uphill battle she faced in getting treatment from white doctors, specifically Dr. Eric Bannec, and nurses in the hospital.
“I had to beg to get the Remdesivir because Dr. Bannec said my chest x-ray was normal. I then had to beg for a CT of my chest.”
Her scan detected pulmonary infiltrates and inflamed lymph nodes, she said, but she continued to wait hours for pain medication. The doctor downplayed her pain, telling her that he felt uncomfortable giving her more narcotics and suggested that she would be discharged.
“Why do I have to prove that there’s something wrong with me in order for my pain to be treated?” “All I know is that I am in intense pain,” “I was crushed. The doctor made me feel like I was a drug addict, and he knew I was a physician.”
She also spoke to a patient advocate who told her nothing could be done. When she asked to be transferred to a different hospital, she was told to just go home.
“I don’t trust this hospital,” Dr. Moore said. “That is not how you treat patients.” “This is how Black people get killed, when you send them home and they don’t know how to fight for themselves.”
Dr. Moore struggled to continue advocating for herself as her condition worsened. The hospital released her on Dec. 7. Twelve hours later, barely able to walk, breathing heavily, with a temperature of 103, BP 80/60, and heart rate of 132, she was taken to a different hospital where she received better care, but the damage had been done. Her condition worsened, she was put on a ventilator, and she died Dec. 20.
Dr. Moore’s case has generated outrage over biased medical treatment of Black patients, particularly when it comes to relieving pain. This problem goes back to the beginning of the war on drugs, over 100 years ago, when drug abuse was equated to minorities. This association is still going on today, with more Blacks being arrested and imprisoned for drug use, even though more whites are involved in drug abuse. The association with drug abuse also affects how blacks are dealt with by law enforcement, with overzealous use of extreme force.
What I want to get across is that all of this could end with the knowledge that drugs are not the cause of drug abuse or addiction, and the repeal of the Controlled Substance Act. The REAL cause of drug abuse is available, if people would just learn it. Systemic racism based on drug use could come to an end.
So what is my macabre reasoning as to what happened to Dr. Moore? Through the 4 years of my researching attacks on doctors, I see a pattern. Dr. Moore was an independent minority physician in an area where the hospital she was a patient in had recently taken over outpatient treatment. In 2015, IU Health added physician offices and multiple urgent care centers. Dr. Moore was therefore a competitor. In my own personal case, I was targeted by the local hospital chain with collusion with the government to take me down. My question is, with Dr. Moore, if the hospital had a vested interest in her death, and she was basically the victim of a “slow code” maneuver. The hospital president and CEO, Dennis M. Murphy, even said he does not believe that his team failed the technical aspects of the delivery of Moore’s care. But “slow codes” are still technically accurate.
If there are any other questionable independent physician deaths in areas of high hospital-owned physician involvement, please send me the information. In my opinion, hospitals owning physicians is not in the citizen’s best interest, and needs to end.
Linda Cheek is a teacher and disenfranchised medical doctor, turned activist, author, and speaker. A victim of prosecutorial misconduct and outright law-breaking of the government agencies DEA, DHHS, and DOJ, she hopes to be a part of exonerating all doctors illegally attacked through the Controlled Substance Act. She holds the key to success, as she can offset the government propaganda that drugs cause addiction with the truth: The REAL Cause of Drug Abuse.
Get a free gift to learn how the government is breaking the law to attack your doctor: Click here to get my free gift
It is not just people of color getting poor treatment, my wife got – what I believe – discriminated against because she was a female and the hospitalist of middle eastern decent and possibly opiophobic … decided that three of her meds to treat her chronic pain – instructed her – IN WRITING AT DISCHARGE D/C those meds COLD TURKEY… she was in the hospital for < 24 hrs and never been seen by this hospitalist before. Our PCP practice – 6 prescribers – was sold to the local hospital about 7-8 yrs ago and then the hospital was sold by a much larger hospital system. now our PCP is not available to see their own pt when they are in the hospital – there are 20 hospitalists on staff at the hospital… here is a lengthy post on this encounter http://www.pharmaciststeve.com/?p=32203
I almost died after a gallbladder surgery because I was labeled by the doctor as a drug seeker, it took them 6 days before taking me in for emergency surgery to fix the problem. I will never go into surgery without a plan that someone will be by my side to help me. It’s not a race it’s a problem with not having empathy for one another, or sometimes doing the right thing. God is the only one that can fix this world.