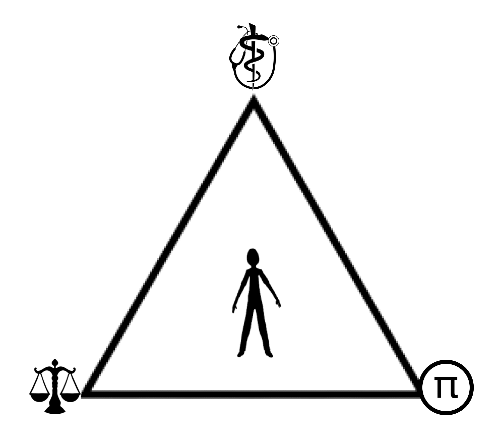
Thousands of years ago three beautiful great schools of human thought and expression were invented and changed the entire world for the better:
- Medicine (the science of improving human mental and physical health)
- Law (the science of rules and punishment to improve the function of societies and human interactions)
- Mathematics (the abstract science of number, quantity, and spaces that describes and explains Nature’s order).
The founders of these sciences were equally impressive. Imhotep (2630–2611 BCE), the first physician created the ideas of Medicine, the oldest of these three sciences. He was later worshipped as the god of medicine in Egypt and in Greece, where he was identified with the Greek god of medicine, Asclepius. Roughly one thousand years later, Law, was invented and developed during the reign of Hammurabi (1792–1750 BCE) of the 1st dynasty of Babylon. Of these three sciences, Mathematics was invented last in 500 BC by the great Greek philosopher, Pythagoras, and is the foundational science of insurance and risk companies that were invented in the relatively modern 1300’s A.D.
Longer lifespans due to technology and science causes more “wear and tear” of the human body’s organs and tissues. Furthermore, trauma caused by modern machinery has caused significant numbers of humans to experience long term chronic pain.
The medical profession as an institution has an important role to play in keeping society functional and efficient. The aim of the medical profession was to return an individual to conventional social roles. If this were not to happen it would have a knock on effect on other institutions and could lead to a breakdown of the social ‘body’. Pain specialists are often consulted to treat damaged tissues by a patient’s primary care doctor who can no longer manage the chronic pain. It is the pain management doctor’s DUTY to research and try unique and unusual treatments to see if it will have a beneficial effect. Therefore, the specialist will read medical journals and attend international and national conferences to learn techniques to help their patients, especially if they are unorthodox and are presented there.
In medical ethics, physicians view their interaction with a patient from either a deontological or teleological philosophy. Teleological (ends justifies the means) philosophy states that if the patient got better (i.e. beneficence and nonmaleficence “do no harm”) then ethically there is no harm of using opiate medications. Deontological philosophy (morality of an action should be based on whether that action itself is right or wrong under a series of rules, rather than based on the consequences of the action), physicians only work for the patient and no other person or entity and therefore has the ethical duty to diagnose and treat the patient to obtain cure or reduce pain and suffering. Physicians do not work for the government as law enforcement officers nor the insurance company and therefore physicians should do their best to help the patient recover even if the treatments are expensive or unpopular. Physicians should not want to “give up” on their patients or their painful diseases and so it is their categorical imperative to try a variety of procedures or medications to try to help the chronic pain patient recover.
This doesn’t mean that physicians do not value patient input and philosophies, “we generally do”, but we often only employ what we have learned during years of training and study. Oftentimes, a physician views the relationship with the patient, as akin to that of a parent and child, with the doctor playing the powerful ‘parental’ role over a passive patient. This is actually where the phrase “patient” comes from, because being a patient required an individual to be passive, trusting and willing to wait for medical treatment, i.e. to literally be ‘patient’. This is how physicians can heal a patient with a chronic disease over time.
The sociologist Talcott Parsons, described patient responsibilities and patient rights which is taught in basic medical ethics courses in medical school. The Rights and Obligations of the patient, according to Parsons’ social model, the sick person can be expected to be afforded two rights, which Parsons called the “Sick Role” in Society. These irrefutable patient rights however were conditional on the patient following two obligations and if these obligations were not met then a patient’s rights as a ‘sick person’ would be withdrawn by society.
The Sick Role patient rights were as follows:
- The sick person is temporarily exempt from performing ‘normal’ social roles, such as going to work or doing household chores, with society affording the patient a greater the exemption from social roles the more severe the disease or sickness.
- Society recognizes that there is a genuine illness which is seen as beyond the control of the sick person and not curable by simple willpower and motivation, and therefore, the sick person should not be blamed for their illness and they should be taken care of by others until they can resume their normal social role.
With the rights of a sick person there are also two obligations:
- The sick person is expected to see being sick as undesirable and so are under societal obligation to try and get well as quickly as possible.
- After a certain period of time, the sick person must seek technically competent help from a doctor and cooperate with the advice of the doctor in order to get better. Damian E M Milton
This is the way medicine has traditionally been taught and practiced. Many doctors and patients are working with one another to appropriately treat chronic pain with opiates. Interestingly many of these internecine struggles between health care providers and insurance companies were foreseen by the leading lawmakers and jurists of the 20th century who were rightfully concerned that insurance/ risk underwriting mathematics companies could become dangerously large enough to dictate health care contrary to Sovereignty of the States who control the medical boards and the healing arts and enacted laws prohibiting the corporate practice of medicine.
THE PEOPLE ex Rel. STATE BOARD OF MEDICAL EXAMINERS v. PACIFIC HEALTH CORPORATION, INC. 12 Cal.2d 156 (1938) enshrined these valid concerns into the annals of law; unfortunately gathering dust, an ineffective deterrent, allowing a present day dystopian nightmare where these mathematics insurance companies view their human clients as “milk cows” on “their plantation”, branded with their insurance logos and member identity cards, paying a contracted health care provider a modest amount of money to keep their “members” healthy enough for a continuous milking stream of premium payments until their clients become too sick, old and costly, relegated to become “beef cows” and consequently denied further expensive, innovative, and experimental health care treatments.
The STATE BOARD OF MEDICAL EXAMINERS v. PACIFIC HEALTH CORPORATION clearly explains the separate functions and responsibilities of physicians and insurance companies quoting: “This doctrine is not challenged by defendant [insurance company], which seeks to distinguish its activities from those previously held to constitute illegal practice of medicine. It is stated that defendant [insurance company] does not itself undertake to perform medical services, but merely to furnish competent physicians; that the contracts do not contemplate that services shall be performed at its offices, but elsewhere; and that the doctors are not employed by defendant on a salary basis, nor directed by defendant, but are compensated for actual services after they are rendered. Defendant’s theory is that the doctors are independent contractors, and that this fact absolves it of the charge of practicing medicine.” It goes on stating, “The evils of divided loyalty and impaired confidence would seem to be equally present whether the doctor received benefits from the corporation in the form of salary or fees.” “This argument ignores the basic policy of the law, of which the statute is merely declaratory, against corporate practice of the learned professions, directly or indirectly.” ; “corporations cannot practice the learned professions.”
Unfortunately, it is inevitable that from time to time the ideas of medicine, mathematics, and law will collide. It seems that there is a great hysteria gripping the nation with respect to opiates. Cooler and logical minds should prevail during this hysteria and lead. We hope the Doctors of Courage will ultimately resolve and provide future legal guidance in Doctor versus Insurance Company versus Law Enforcement disputes and the increasingly common “turf” battles concerning the Practice of Medicine by learned professionals and physicians, from the malignant encroachment of mathematics based, risk underwriting companies, or law enforcement officers masquerading as “back seat driving” health care providers.
Doctors of Courage must lead the rest of the nation in the effort to defend physicians who treat chronic pain patients without fear of reprisal from insurance companies or law enforcement. We look forward to your leadership. Godspeed!
With Greatest Respect,
Blue Lotus M.D.
The Author received an honorable discharge from the U.S. Navy where he utilized regional anesthesia and pain management to treat soldiers injured in combat at Walter Reed Hospital. The Author is passionate about medical research and biotechnological innovation in the fields of 3D printing, tissue engineering and regenerative medicine.